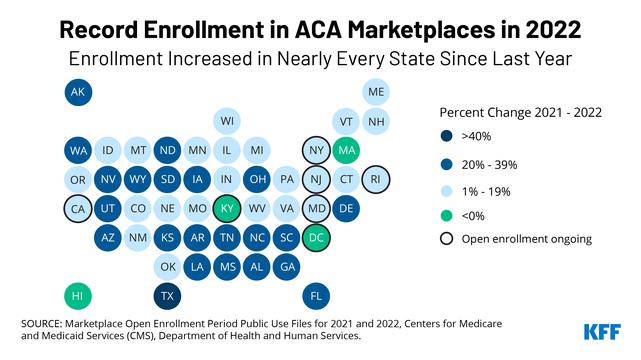
Even as the ninth annual Open Enrollment period gets underway, the Affordable Care Act (ACA) Marketplaces continue to evolve and important changes are expected.Keep an eye on:
1. Open enrollment dates are changing
In most states, the Open Enrollment period will be longer this time.In recent years, in the HealthCare.gov states, it has lasted only 6 weeks; but now it will run from November 1, 2021 through January 15, 2022.That said, people should still sign up by December 15 if they want coverage to take effect on January 1.Signing up later generally means coverage will start February 1. State-run marketplaces have flexibility to hold even longer OE periods and some will do so.
2. Plan choices and premiums will change in 2022
As happens every year, premiums for marketplace plans will change somewhat in 2022.In HealthCare.gov states, the average benchmark plan premium will be about 3% lower than in 2021, while in some state-based marketplaces, qualified health plan premiums will increase modestly, on average.
In addition, the number of insurers participating in the marketplace will increase in 2022.In HealthCare.gov states, 32 additional insurers will offer marketplace coverage, bringing the total to 213.Competition by insurers can sometimes change the so-called benchmark plan (the second-lowest cost silver plan, on which marketplace subsidies are based) if a new silver plan earns this designation in 2022.On average, consumers in HealthCare.gov states will have a choice of nearly 83 qualified health plans in 2022, compared to an average of 46 plans in 2021.
3. Improved marketplace subsidies continue and will reduce net premiums for most consumers
Expanded marketplace premium subsidies, enacted under the American Rescue Plan Act (ARPA), took effect in 2021 and remain in effect for 2022.The dollar amount of premium tax credits increased and now fully cover the cost of enrolling in the benchmark silver plan for consumers with income up to 150% FPL.Before, consumers at 150% FPL had to pay more than 4% of household income for the benchmark plan. For people up to 150% FPL, cost sharing subsidies also substantially reduce deductibles and copays under zero-premium silver plans, making them similar to platinum plans.
ARPA also extended eligibility for premium tax credits to reach people with income over 400% FPL ($51,520 for a single person in 2022, $87,840 for family of 3).Now these consumers must contribute no more than 8.5% of income toward the benchmark silver plan.Before, for older consumers, the age-rated premium for benchmark plans could easily cost more than 20% of household income.ARPA premium tax credit changes are temporary, ending after 2022, although legislation to make them permanent is pending in Congress.
The KFF subsidy calculator helps people estimate the amount of financial assistance based on their age, income, family size, and zip code.
4. Active renewing is strongly recommended
In most states, if enrollees have not updated their application and plan selection for 2022, the marketplace may auto-re-enroll them in their current plan or a similar plan for the coming year.Over the last three Open Enrollment periods, about 40% of returning marketplace participants were auto-re-enrolled. However, passively renewing can sometimes put consumers at a disadvantage.For example, if the benchmark plan changes from one year to the next (e.g., due to entrance of new insurers), the dollar value of tax credits, which are tied to the cost of the benchmark plan, can also change.That means someone now enrolled in the 2021 benchmark plan who is passively renewed could see unexpected monthly premium cost increases if another plan gains benchmark status in 2022 and costs less.
Enrollees who did not take advantage of new ARPA subsidies when those subsidies came online this year could also miss out if they don’t actively renew.While the marketplace automatically adjusted subsidies for many current enrollees at the end of the COVID-SEP, it could not apply more help to people already in zero-premium bronze plans.More than 800,000 HealthCare.gov enrollees were in zero-premium bronze plans at the end of Open Enrollment for 2021, and many of them would be better off in silver plans with the new ARPA subsidies.All marketplace enrollees are encouraged to update their application during Open Enrollment, even if personal circumstances have not changed, so they can see all current plan and financial assistance options. Otherwise, the extended Open Enrollment will leave a short window (until January 15) when consumers can still make changes.
5. People with very low income will have added time to enroll
Starting in 2022, HealthCare.gov will allow enrollment throughout the year for people with income up to 150% of the federal poverty level (or FPL, which is $19,320 per year for a single person in 2022, $32,940 for family of 3).A new special enrollment opportunity will be offered each month, and as noted above, plan choices will include zero-premium plans with vastly reduced deductibles.To sign up during the year, people can attest to having 2022 income at or below 150% FPL, then continue with their application.The marketplace will conduct real-time income verification, as it does for all applicants, and might ask for additional documentation to be submitted within 90 days.This year, HealthCare.gov will ask for documentation when consumers estimate their 2022 income will be substantially lower (by 50% or $12,000, whichever is greater) than the amount reported on their most recent federal income tax return.
Extended enrollment could benefit millions of people.At the end of the last Open Enrollment, roughly 1/3 of marketplace participants had income at or below the 150% FPL threshold; and during the recent COVID enrollment opportunity in 2021, 45% of people signing up in HealthCare.gov states (22% in state marketplaces) had incomes at or below this threshold. Open Enrollment remains the best time to sign up for year-long coverage, but the added enrollment opportunities will make it easier for people to sign up for premium-free plans with low cost-sharing throughout the year.
6. More enrollment help will be available
In HealthCare.gov states, funding for Navigators has been restored following years of substantial funding cuts averaging 84%.Navigators are trained enrollment experts, certified by the marketplace, who provide free help to individuals shopping for marketplace coverage and subsidies, or help signing up for Medicaid and CHIP. Twice as many programs will be available in 2022, with more resources to serve consumers, including extended hours, remote assistance, and language translation services.The “Find Local Help” link on HealthCare.gov provides contact information and hours of operation for the nearest programs.
7. Three new state-run marketplaces will open
This fall 3 states – Kentucky, Maine, and New Mexico – are launching state-based marketplaces.Some 173,000 residents of these states already enrolled in plans through HealthCare.gov will have their data transferred to the new state marketplace and receive instructions for accessing their accounts and enrolling in 2022 coverage.
8. New surprise medical bills protection will take effect
Most marketplace plans are HMOs or EPOs with closed provider networks, meaning they generally will not cover non-emergency care from an out-of-network provider; and even when plans do cover out-of-network claims, consumers can face “balance billing” charges in excess of what their plan will pay. That will change next year when a new federal law starts protecting consumers from surprise medical bills.Beginning January 1, all insurance plans, including marketplace plans, must cover emergency services (other than ground ambulance) at the in-network rate, and out-of-network emergency room facilities and doctors will not be allowed to bill patients more than the in-network cost sharing amount under their plan.These protections will also apply for non-emergency care received by patients while at in-network hospitals, ambulatory surgery centers, or other facilities.
9. Some recent changes have changed back
This year, it will again be important for consumers to carefully estimate their 2022 income when they apply for marketplace subsidies.Thanks to a temporary repayment holiday enacted as part of pandemic relief legislation, people who filed their 2020 tax return this spring did not have to repay any excess 2020 premium tax credit; but the repayment requirement is now back in force.Marketplace consumers who under-estimate their 2022 income risk owing more taxes if they claim excess premium tax credits during the year.If people do experience a significant change in their 2022 income after they’ve signed up, they should update their marketplace account as soon as possible to avoid receiving excess subsidies.
Another key change this year reversed Trump Administration revisions to the “public charge” rule that would have made it harder for immigrants to enter or stay in the U.S. if they needed public assistance to obtain health coverage.That action deterred many people from applying for or remaining enrolled in health coverage for fear this could impact their immigration status.This year the Biden Administration rescinded the Trump Administration changes to the public charge rule.Now, under current rules, immigration officials will not consider enrollment in Marketplace, CHIP, or Medicaid coverage as part of a public charge test when people apply for a green card.
10. Will New Enrollment Records Be Set?
Marketplace enrollment reached a record high of 12.2 million people as the special COVID enrollment period ended in most states in August 2021.Affordability gains due to expanded subsidies, as well as outreach and enrollment assistance, likely contributed to this result.Even so, an October 2021 KFF poll found that only 1 in 4 people who are uninsured or who buy their own health insurance checked to see if they qualified for more help once the ARPA subsidy improvements became available.Shortly after ARPA’s enactment, KFF estimated nearly 11 million uninsured Americans were eligible for but not enrolled in subsidized marketplace plans, including 1.4 million who became newly eligible for marketplace subsidies.These uninsured individuals, including those eligible for zero-premium plans, disproportionately have a high school education or less, are Hispanic, young adults, live in rural areas, or lack Internet access at home. It remains to be seen during this next Open Enrollment whether additional time and enrollment help, and expanded financial help yields even more signups.